The US Gov. Health Statistics Agency Directs Hospitals to Confirm Suspected COVID-19 Deaths As Confirmed
While the hysteria and panic over COVID-19’s presumed lethality grow, so do serious questions about whether the government and media are accurately reporting on the scale of the threat. A document has surfaced revealing that the government’s own health statistics agency is now directing hospitals to define deaths merely suspected to be linked to COVID-19 as confirmed on death certificates.
[Update: on April 5th, the WHO posted ICD guidelines revealing that only “probable” or “suspected” cases of COVID-19 can be written as confirmed causes of death, and where virus testing is inconclusive.]
The National Vital Statistics System (NVSS), an inter-governmental system of sharing data on the vital statistics of the population of the United States, which coordinates different state health departments of the US states and the National Center for Health Statistics, a division of the Centers for Disease Control and Prevention, released a statement on March 24th announcing a new ICD code for COVID-19 deaths.
The NVSS statement (full release in text and screenshotted below) directs those recording death certificates to identify the cause of death to be COVID-19 even when it is only “assumed to have caused or contributed to death”:
“Should “COVID-19” be reported on the death certificate only with a confirmed test?
COVID-19 should be reported on the death certificate for all decedents where the disease caused or is assumed to have caused or contributed to death. Certifiers should include as much detail as possible based on their knowledge of the case, medical records, laboratory testing, etc. “
The NVSS directives also reveal that they are not likely to pursue confirmation of these cases in the future:
“…If the death certificate reports terms such as “probable COVID-19” or “likely COVID-19,” these terms would be assigned the new ICD code. It Is not likely that NCHS will follow up on these cases.”
This indicates that so-called “confirmed COVID-19 deaths” reported through national health databases and the media at large are, in fact, not being confirmed. Here is the full release:
“COVID-19 Alert No. 2
March 24, 2020
New ICD code introduced for COVID-19 deaths
This email is to alert you that a newly-introduced ICD code has been implemented to accurately capture mortality data for Coronavirus Disease 2019 (COVID-19) on death certificates.
Please read carefully and forward this email to the state statistical staff in your office who are involved in the preparation of mortality data, as well as others who may receive questions when the data are released.
What is the new code?
The new ICD code for Coronavirus Disease 2019 (COVID-19) is U07.1, and below is how it will appear in formal tabular list format.
U07.1 COVID-19
Excludes: Coronavirus infection, unspecified site (B34.2)
Severe acute respiratory syndrome [SARS], unspecified (U04.9)
The WHO has provided a second code, U07.2, for clinical or epidemiological diagnosis of COVID-19 where a laboratory confirmation is inconclusive or not available. Because laboratory test results are not typically reported on death certificates in the U.S., NCHS is not planning to implement U07.2 for mortality statistics.
When will it be implemented?
Immediately.
Will COVID-19 be the underlying cause?
The underlying cause depends upon what and where conditions are reported on the death certificate. However, the rules for coding and selection of the underlying cause of death are expected to result in COVID- 19 being the underlying cause more often than not.
What happens if certifiers report terms other than the suggested terms?
If a death certificate reports coronavirus without identifying a specific strain or explicitly specifying that it is not COVID-19, NCHS will ask the states to follow up to verify whether or not the coronavirus was COVID-19. As long as the phrase used indicates the 2019 coronavirus strain, NCHS expects to assign the new code.
However, it is preferable and more straightforward for certifiers to use the standard terminology (COVID-19).
What happens if the terms reported on the death certificate indicate uncertainty?
If the death certificate reports terms such as “probable COVID-19” or “likely COVID-19,” these terms would be
assigned the new ICD code. It Is not likely that NCHS will follow up on these cases.
If “pending COVID-19 testing” is reported on the death certificate, this would be considered a pending record. In this scenario, NCHS would expect to receive an updated record, since the code will likely result in R99. In this case, NCHS will ask the states to follow up to verify if test results confirmed that the decedent had COVID- 19.
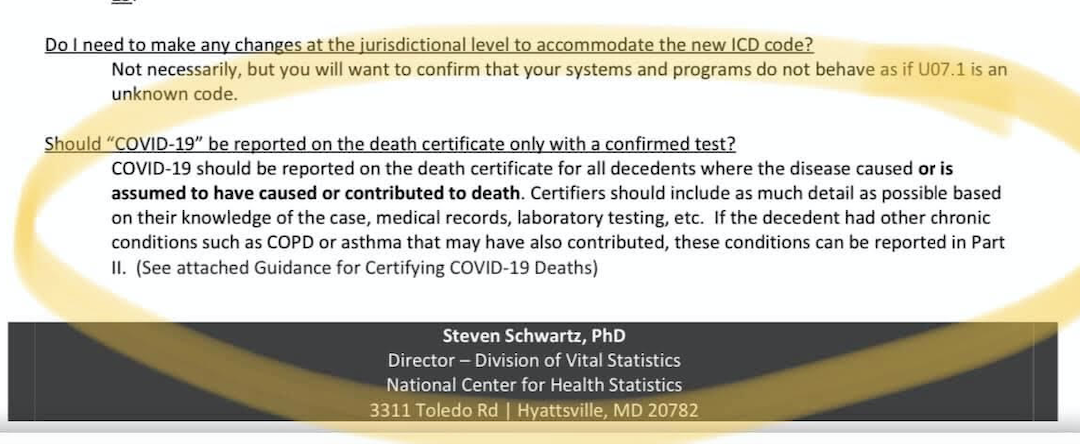
Do I need to make any changes at the jurisdictional level to accommodate the new ICD code?
Not necessarily, but you will want to confirm that your systems and programs do not behave as if U07.1 is an unknown code.
Should “COVID-19” be reported on the death certificate only with a confirmed test?
COVID-19 should be reported on the death certificate for all decedents where the disease caused or is assumed to have caused or contributed to death. Certifiers should include as much detail as possible based on their knowledge of the case, medical records, laboratory testing, etc. If the decedent had other chronic conditions such as COPD or asthma that may have also contributed, these conditions can be reported in Part
II. (See attached Guidance for Certifying COVID-19 Deaths)
Come Follow Us on Twitter – Come Like Us on Facebook
Check us out on Instagram – And Sign Up for our Newsletter


.jpg)